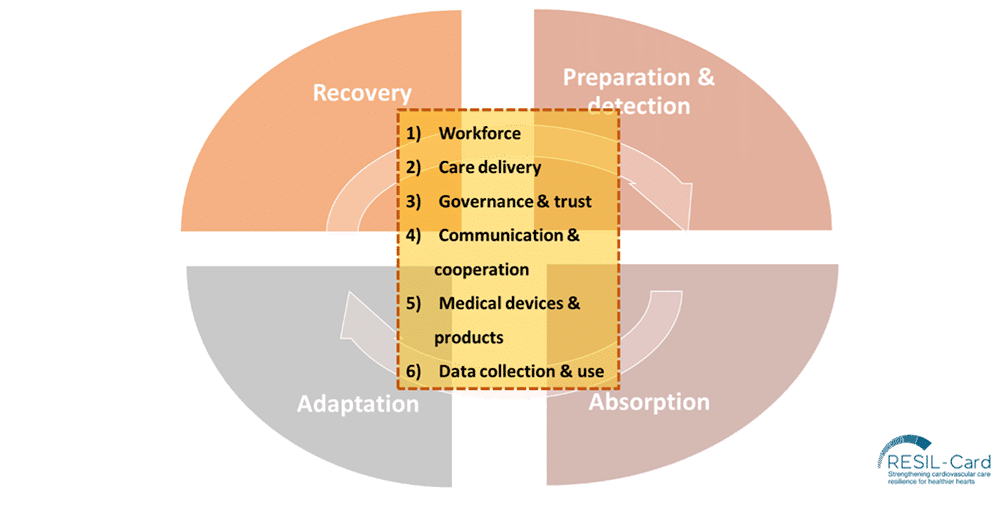
The RESIL-Card survey aimed to capture the experiences of healthcare professionals involved in the cardiovascular (CV) care pathway during the COVID-19 pandemic. It was designed around six key dimensions of health system resilience: workforce, care delivery, governance and trust, communication and cooperation, medicals devices and products, and data collection and use (Figure 1).

The RESIL-Card survey aimed to capture the experiences of healthcare professionals involved in the cardiovascular (CV) care pathway during the COVID-19 pandemic. It was designed around six key dimensions of health system resilience: workforce, care delivery, governance and trust, communication and cooperation, medicals devices and products, and data collection and use (Figure 1).
The survey was conducted in May-June 2024 and targeted interventional cardiologists, nurses and allied professionals in the 27 EU Member States and Ukraine, specifically members of the “PCR Companions” network. The survey was disseminated to a potential audience of 4,657 professionals, supplemented by outreach through social media and scientific conferences.
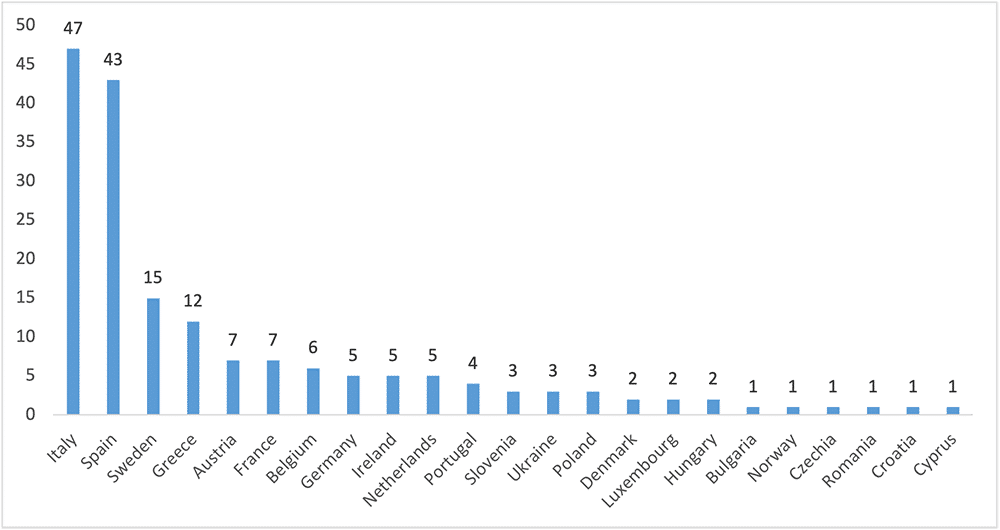
A total of 177 responses were collected. Physicians made up 92% of respondents (n=163), primarily interventional cardiologists (n=124), with fewer responses from nurses (7%, n=13) and allied professionals (1%, n=1). Most of respondents were men (60%, n=107) and worked in public hospitals (85%, n=153). Most responses came from Italy (n=47) and Spain (n=43) (Figure 2).
Before the COVID-19 pandemic, key challenges identified were shortages in infrastructure capacity and healthcare professionals. During the pandemic, key findings across the six dimensions of resilience included:
a) Workforce: the measures considered most helpful to minimise care disruptions were the reorganisation of clinical teams, reallocation of health staff, flexible nursing teams, and increasing digitalisation.
b) Care delivery: shortages in infrastructure, especially intensive care unit (ICU) beds, were commonly reported. Solutions included devising new infrastructures, repurposing existing ones, and fostering national and international collaborations among ICU units. Diagnostic delays, particularly for trans-oesophageal echocardiogram and cardiovascular magnetic resonance imaging, were frequent. Elective diagnostic catheterisation procedures faced wait times pressure. Innovations such as teleconsultations, shorter hospital stays and home-monitoring systems emerged as common in new care delivery models.
c) Governance and trust: Decision-making was most frequently led by hospital managers, cardiology department heads, and heart teams.
d) Communication & cooperation: Changes in referral policies, such as between primary and secondary care, and new communication channels to inform patients were frequent.
e) Medical devices & products: The most frequently reported shortages concerned mechanical ventilators.
f) Data collection & use: About half of the respondents reported that their hospitals had data systems in place to track the volume of cardiac patients treated.
Looking to the future, respondents identified several priorities to improve resilience: protecting healthcare workers, enhancing the adaptability of hospital infrastructures, involving healthcare professionals in decision-making, improving patient and inter-organizational communication, and advancing digitalisation and data utilisation.
The RESIL-Card Consortium would like to express gratitude to the cardiologists and nurses who have contributed to the cognitive testing of the RESIL-Card survey with their time and expertise, whose invaluable insights were instrumental in refining the survey before its release. We extend our heartfelt gratitude to all participants of the survey, who provided us with relevant insights from the field, which will be key to advance the RESIL-Card project.